Today's slightly complex post from clinicalpainadvisor.com (see link below) looks at the findings of Dr. Forest Tennant, that he presented at a recent Pain Week conference. His conclusions that neuropathic pain is the body's response to massive inflammation of the nervous system will come as little surprise to neuropathy patients whose symptoms scream 'inflammation'. However, you may not be as aware of his ideas, that hormone therapy may be the answer. He claims that hormonal treatment may suppress that inflammation and that there is enough research to bear that out. However, pharmaceutical companies are not exactly falling over themselves to develop practical treatments because hormones can't be patented and therefore, profits can't be made. So where does that leave us long-suffering nerve pain patients? If Dr Tennant is right and neuro-hormones are a proven answer to neuropathic pain, then we still can't roll up at the doctor's practice and ask for them because plainly they don't yet exist as marketable therapies. More research and clinical trials are necessary but who's going to finance them if there's no profit to be made! Same old story eh!!
Neuroinflammation: Treating the Underlying Cause of Chronic, Severe Pain
Tori Rodriguez, MA, LPC September 08, 2017
“Neuroinflammation due to microglial activation is the underlying cause of severe persistent or constant pain,” pointed Dr Tennant.
The following article features coverage from PAINWeek 2017 in Las Vegas, Nevada. Click here to read more of Clinical Pain Advisor's conference coverage.
LAS VEGAS – At Pain Week 2017, held September 5-9, Forest Tennant, MD, DrPH, an internist, addictionologist, and researcher at the Veract Intractable Pain Clinics in West Covina, California, sought to highlight the role of neuroinflammation in severe chronic pain.1
Dr Tennant aimed to help attendees identify patients with neuroinflammation, the diseases most commonly implicated in severe neuroinflammation, complications and outcomes associated with the condition, and optimal treatment options. “Neuroinflammation due to microglial activation is the underlying cause of severe persistent or constant pain, and unless it is suppressed, no real treatment of the cause of pain can be realized,” Dr Tennant told Clinical Pain Advisor.2,3
“Time has taught us that there is a relatively short list of pathologic conditions that cause the most severe, chronic pain — every pain practitioner should have awareness of these,” he added. These conditions include Ehlers-Danlos syndrome, sickle cell disease, Lyme disease, and severe peripheral neuropathies. Dr Tennant also gave examples of pathologic consequences and symptoms of neuroinflammation, including constant pain, insomnia, depression, central sensitization with allodynia and hyperalgesia, and febrile heat episodes.
Physical examination findings may include elevated pulse rate, respiratory rate, blood pressure, and reflex activity; cold extremities; mydriasis; and diaphoresis. Diagnostic tests may reveal elevated serum levels of inflammatory markers such as high-sensitivity C-reactive protein, interleukins, and tumor necrosis factor, as well as abnormal levels of hormones such as dehydroepiandrosterone, testosterone, and progesterone.
Here are the 4 components of treatment for centralized pain and neuroinflammation:
Pain relief using standard nonpharmacologic and pharmacologic approaches
Neuroinflammation control with varying combinations of low-dose corticosteroids, anti-inflammatories, microglial suppressors, and nutritional supplements
Spinal fluid flow exercises including walking arm swings, upper body gyration, and deep breathing
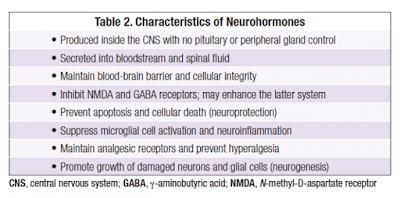
Neuroregeneration with B12, replenishment of hormones showing low serum levels, and the administration of neurohormones that have been found to produce neuroregeneration in animal studies — for example, oxytocin, human growth hormone, and human chorionic gonadotropin4
According to Dr Tennant, there is a large body of animal and in vitro research on neuroregeneration and hormonal suppression of neuroinflammation, and results have been positive among the few clinical researchers who have applied the basic science findings to real patients. He recommends clinical trials with neurohormones in motivated patients whose pain is reasonably under control. “It is too early to recommend a specific clinical indication, but the neurohormones appear quite safe and I believe astute practitioners should begin using neurohormones,” he added.
Related Articles
Diabetic Peripheral Neuropathic Pain: Evaluating Treatment Options
Updated Diagnostic Criteria for Neuropathic Pain in SCI, Stroke, MS
Neuropathic Pain in Low Back-Related Leg Pain: the State of Evidence
Risks Associated With Neuropathic Pain Treatment
He stated that neither FDA approval of these agents nor a consensus on evidence-based practice in this area is likely, as pharmaceutical companies will not spend money on large trials since hormones cannot be patented, and they have not been in use long enough to accumulate much evidence-based data. He distributed references to give practitioners confidence that prescribing neurohormones is not a “pie-in-the-sky” concept.
“Overall, hormone treatment of both types should begin to be a new paradigm in pain treatment,” Dr Tennant said. “To date, we've been simply throwing symptomatic pharmaceuticals at pain patients because that is all we have had — now we can begin to treat the underlying cause of pain as opposed to just symptomatic care.”
Disclosures Dr Tennant is Editor in Chief of the journal Practical Pain Management, and is a speaker for Regenesis Biomedical.
Read more of Clinical Pain Advisor's coverage of PAINWeek 2017 by visiting the conference page.
References
Tennant F. Neuroinflammation: treating the underlying cause of chronic, severe pain. Presented at Pain Week 2017; September 5-9, 2017; Las Vegas, NV.
Graeber MB, Christei MJ. Multiple mechanisms of microglia: a gatekeeper's contribution to pain states. Exp Neurol. 2012; 234(2):255-61. doi:10.1016/j.expneurol.2012.01.007
Gwak YS, Hulsebosch CE. Remote astrocytic and microglial activation modulates neuronal hyperexcitability and below-level neuropathic pain after spinal injury in rat. Neuroscience. 2009;161(3):895-903. doi:10.1016/j.neuroscience.2009.03.055
Lei ZM, Rao CV. Neural actions of luteinizing hormone and human chorionic gonadotropin. Semin Reprod Med. 2001;19(1):103-9. doi:10.1055/s-2001-13917
http://www.clinicalpainadvisor.com/painweek-2017/chronic-and-severe-pain-often-accompanied-with-neuroinflammation/article/685529/
No comments:
Post a Comment
All comments welcome but advertising your own service or product will unfortunately result in your comment not being published.